Understanding the potential of leptomeningeal collaterals in stroke
Exploring the unique mechanism of this collateral circulation in stroke.

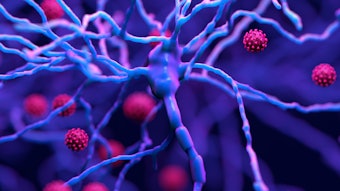
The leptomeningeal collaterals comprise a secondary blood flow route to avert, limit injury and aid reperfusion in ischemic stroke. These tiny arterial anastomoses (50-100 microns), spreading across the surface of the brain, can connect the territories of the main vessels, including the middle, anterior and posterior cerebral arteries.
The LMCs, also known as pial collaterals, are the heroes of moyamoya syndrome, a progressive stenosis of the intracranial internal carotid arteries and their proximal branches. In this condition, almost the entire blood flow to the brain is fed via the LMCs in this setting.
“The real question is, how do we achieve that therapeutically?” said  David S. Liebeskind, MD
David S. Liebeskind, MD
That is the subject of Wednesday’s session, “The Leptomeningeal Collaterals: Understanding Their Specialized Function and Regulation in the Context of Stroke,” moderated by Liebeskind.
As collateral circuits go, the LMCs are anatomically and functionally different than other collateral circulation.
“The LMCs are interesting because except for a few other places in the body, they don’t exist anywhere else, and specifically they are very different than the collaterals that exist in the heart and to a large degree to the collaterals that exist in the peripheral arterial circulation as well,” said Liebeskind, who has studied the clinical relevance and impact of collateral circulation in acute ischemic stroke and intracranial atherosclerosis over the last 20 years.
The tiny anastomoses form selectively between the terminal limits or downstream branches of the arterial territory and the adjacent territory. “They allow the blood flow to go from one territory across a small connection and effectively backward into the other arterial territory,” said Liebeskind. “This retrograde or reverse arterial flow occurring in the downstream branches of a main arterial tree happens because there’s a blockage upstream in that vessel and the pressure drops. When it occurs in reverse fashion, the blood flow comes in through a few smaller vessels and then starts coursing toward the larger branches and trunks of that blocked arterial territory.”
The sudden increase in blood flow across small vessels causes an increase in shear stress, which effectively acts as a trigger to dilate the LMCs, consequently decreasing shear stress and increasing blood flow, he said.
“There are a lot of molecular mechanisms involved in terms of what gets triggered when this occurs, said Liebeskind. “In other words, it’s not just the physical forces, as you actually cause a leakiness of the LMCs at this level that allows them to dilate, to loosen their structure in the vessel wall and dilate outward.”
The session will focus on basic science research in LMCs. “The two principal avenues that have been attempted in animal models are either through increasing pressure at one end, or alternatively, attempting to dilate those blood vessels,” said Liebeskind.
Four science presentations will cover mechanisms of LMC dilation in response to stroke in young and aged mice, mechanisms of collateral failure in stroke, the modification of LMC function in hypertension and dysregulation of LMC function in models of Alzheimer's disease.
Much is yet to be learned about the tiny, yet mighty leptomeningeal collaterals and their role in stroke.