Overhauling traditional random clinical trials
Pursuing innovative solutions could improve efficiency, inclusivity and patient care.

Clinical research faces stiff headwinds. Trials are growing costlier. The questions they address are trickier. Recruitment can be slow. And greater inclusivity is essential.
But adaptation and innovation will help stroke scientists meet the moment, speakers at ISC say.
Although traditional methodologies in randomized clinical trials (RCTs) increasingly face hurdles, innovative solutions to enhance the design and execution of stroke trials exist, according to Nishita Singh, MD, an assistant professor of neurology at the University of Manitoba in Winnipeg.
“RCTs are struggling to keep pace with evolving needs. The clinical questions we face today are far more complex than before,” Singh said.
“For example, we need to address tailored interventions for patients with unique characteristics, such as those with minor strokes, unusual clot locations or co-existing conditions like pre-morbid disability or cognitive impairment. These situations often require trial designs that traditional RCTs are not equipped to handle efficiently.”
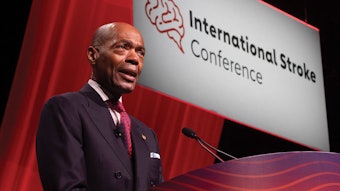
Singh is among the speakers Wednesday at the session “Modernizing Stroke Trials for the 21st Century: Scale, Strategy, and Technology.” Her presentation, “Innovative Consent Methodologies in Stroke Trials,” will explore how neurologists can rethink the consent process to meet the challenges of acute stroke trials.
Traditional informed consent approaches are impractical because of the critical time window in stroke research. Alternatives such as deferred consent, waiver of consent and advance consent models prioritize ethical integrity while addressing logistical realities, Singh said. These innovations can streamline trial operations, improve recruitment and maintain ethical rigor, she said.
Recruiting larger, more diverse study populations is another key challenge. Historically, RCTs have excluded groups including women, the elderly and patients from underrepresented regions, which limits the applicability of findings on a global scale. And conducting large-scale, multinational trials is increasingly expensive, with regulatory hurdles, site training and data harmonization adding to the logistical burden.
“As we tackle these challenges, it’s clear that traditional models must adapt to stay relevant,” Singh said.
Several promising solutions are on the horizon, Singh said. For example, adaptive trial designs allow researchers to make real-time adjustments based on interim results, such as modifying sample sizes or adding treatment arms. This flexibility accelerates timelines and reduces costs, she said.
Technology is another game-changer.
“The use of telemedicine for remote recruitment and follow-ups has proven invaluable, especially in the wake of the pandemic,” Singh said. “Additionally, AI-driven data analytics can help us predict patient outcomes and stratify treatments more effectively.”
There are other innovative solutions, according to Tolulope Sajobi, PhD, a professor of biostatistics at the University of Calgary Cumming School of Medicine in Alberta. These include integrating wearable devices for long-term and rich data collection (global harmonization and standardization of data); linking multiple data sources (such as electronic health records, registries and omics data); and leveraging digital health platforms for enrollment and outcome assessment.
Investing in modern data infrastructures that ensure flexible outcome assessment and data management is critical — and cost-effective — for generating robust evidence about the efficacy and effectiveness of interventions, said Sajobi, whose presentation Wednesday is titled “Modernizing Data Infrastructure for Large Global Trials.”
“Prioritizing patient-centered data collection and infrastructures that simplify outcomes assessment while providing participants with flexibility to complete their outcomes from anywhere in the world will improve the inclusivity of trials,” he said.
In addition, engaging patients in the design phase of trials can ensure that protocols are relevant and feasible, Singh and Sajobi said.
“By embracing these innovations, we can make stroke trials more efficient, inclusive and impactful, ultimately improving care on a global scale,” Sajobi said.